In vivo Reprogramming
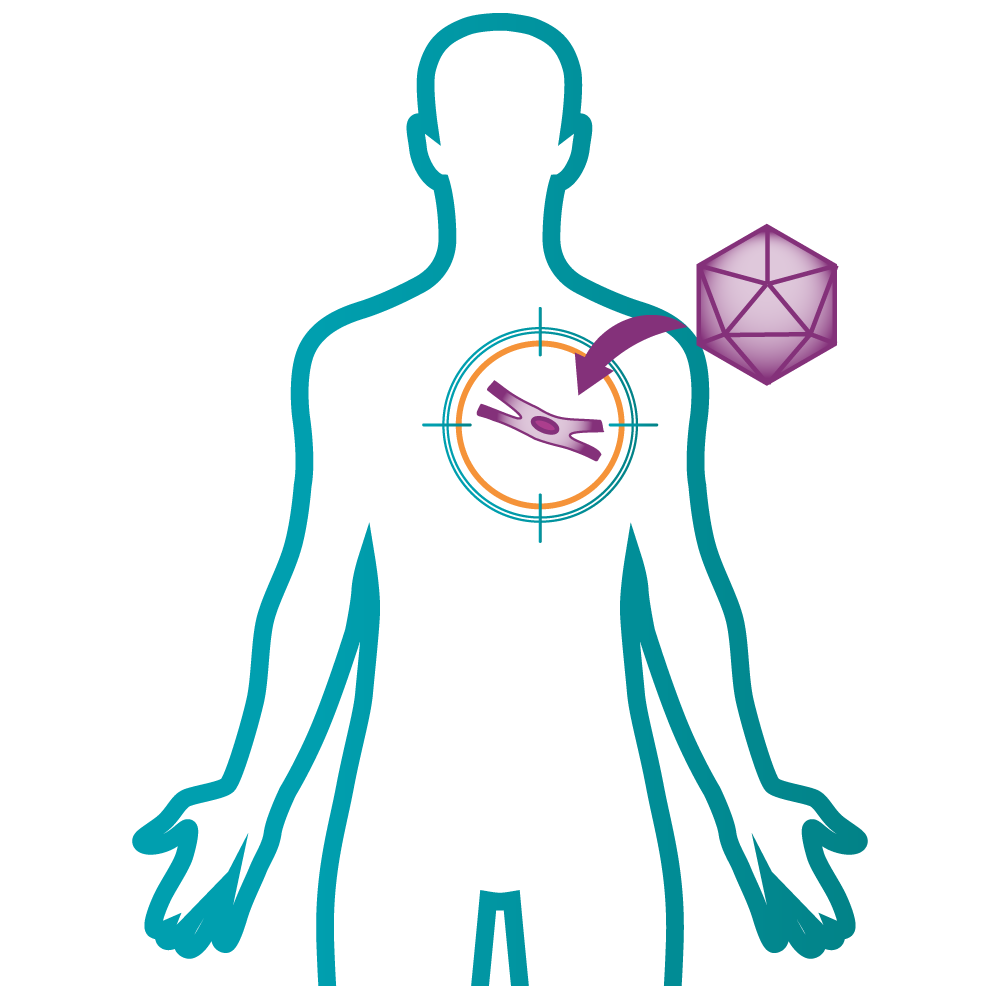
In vivo reprogramming is a therapeutic approach to regenerative medicine aimed at delivering a cell-based therapy to an organ or tissue in need of functional restoration without the use of a cellular agent. Building on principles of cellular reprogramming, epitomized by Yamanaka’s Nobel-winning discovery of ‘Induction of Pluripotent Stem Cells from Adult Human Fibroblasts by Defined Factors’ in 2007, in vivo reprogramming employs transdifferentiation, or direct conversion of a source cell type into a target cell type without an intermediate pluripotent or stem cell stage, to affect the conversion of cells directly in the human body.
The rationale for in vivo reprogramming arises from the bottlenecks associated with the development of ex vivo cell therapies – manufacturability, scalability and the risk of immune rejection. Despite progression toward allogeneic development, the need to replicate the cell’s in vivo microenvironment in in vitro conditions and process variation between cell type, indication or disease area will remain a challenge.
In vivo reprogramming leverages the plasticity of cells and methods for the induction of cellular identity genes, such optimal combination of transcription factors, to achieve cellular reprogramming directly in situ, whilst harnessing the innate microenvironment to maintain functional maturity. The method has the potential to circumvent the need for ex vivo cell manufacture and the risk of immune rejection. Research into in vivo reprogramming methodologies includes the in situ generation or rejuvenation of cardiomyocytes, pancreatic β cells and neurons for regenerative medicine, as well as muscle regeneration and rejuvenation/anti-aging studies via partial reprogramming using the OKSM factors.